In this topic you will learn how to complete the first part of the mobility assistive products screen.

If you haven’t already, download and print copies of the:
If you are unable to download the form, don’t worry. Each of the questions on the form are clearly shown as you go through the module.
TAP Mobility assistive products screen form
The mobility screen form is a simple tool that can be used as a guide during screening.
The form includes questions to ask a person with mobility difficulties to help you find out:
- If the person may benefit from the mobility assistive products included on the screen form
- If a referral to a health care professional, rehabilitation service, prosthetic and orthotic service or other assistance is needed.
Whenever you see this icon on the form, it means that the person may need referral.
This screen focuses on mobility devices. However, a person who uses a mobility device may also benefit from other types of assistive products.
At the end of the form, there is space to write notes and make a plan for the person.
Let’s go through each part of the mobility screen now.
Information about the person
Start by collecting general information about the person, including their contact details, gender and age.
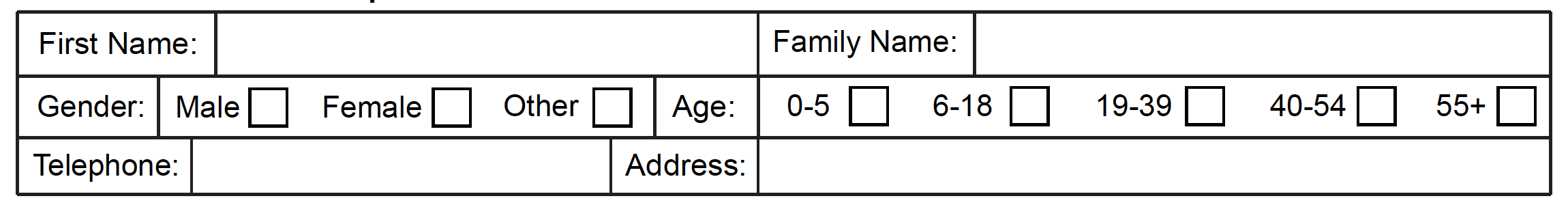
Simple mobility and health risk check
Before providing a mobility device, it is important to check for any mobility or health risks that may need further investigation and/or management.
Use this part of the screening form to find out if the person has a mobility or health risk.
Sudden loss of mobility
Ask the person:
Has your mobility reduced a lot in the past three months?
![]()
A sudden loss of mobility, can be a sign that a person has a health condition that needs to be assessed and treated.
Refer to a health and/or rehabilitation professional for further advice.
The person may still benefit from a mobility device, so complete the screen.
Reflection
Can you think of anyone you know who suddenly became unhealthy or lost their mobility?
Did they have a health condition (illness)?
Children’s mobility
Ask parents or carers of young children:
Is the child older than two and has not yet begun to walk?
![]()
By the age of two many children are able to walk on their own.
If a child is over two and not yet walking, discuss referral to a health professional or rehabilitation service.
Early referral gives the best opportunity to develop a child’s abilities.

Risk of falling
Ask the person:
Do you worry about falling over, or do you fall often?
![]()
If the person has balance problems, they may worry about falling over.
Falling is particularly dangerous for older persons. They are more likely to injure themselves and take longer to recover.
The risk of falling can be increased by problems such as difficulty seeing or hearing, difficulty thinking and remembering, being frail and difficulty with balance.
If an older person has fallen more than once in the past 12 months, they are at risk of falling again.
Discuss with them whether a mobility or other assistive product would help to prevent them from falling.
You may also refer them to a rehabilitation service for a full falls assessment.

Remember Sofia?
Sofia is 68 years old and recently had a few falls in her home. After an assessment, Sofia was given a rollator to help her move around. She has enjoyed walking to the local shops. However, Sofia then had another fall going to the toilet at night.
Activity
Which actions below would be helpful for Sofia?
Correct
A rehabilitation service could provide exercises to help Sofia improve her strength, balance or coordination. The service could also give Sofia advice about making her environment as safe as possible to prevent more falls.
Correct
A grab bar may help Sofia stand up and balance when getting out of bed.
Correct
She may have a need for other assistive products – for example; difficulties seeing or hearing reduce balance and increase the risk of falling, a personal alarm can alert help if Sofia falls and cannot get up.
Pressure wounds
A pressure wound is a breakdown of the skin. It is usually over a bony area such as the back, hips or seat bones.
Pressure wounds are a common problem for people with loss of feeling (sensation) or difficulty moving and changing position.
If someone has had a wound before they are at risk of another wound.
Look at these pictures of pressure wounds which show how a wound can begin as a mark and progress to becoming larger, deeper and possibly infected.
On darker coloured skin the first stage of a wound may be hard to see. Check whether the skin feels hotter and/or swollen than the surrounding area.
On light coloured skin a mark will appear red. On darker coloured skin a mark may be a blue or purple colour.
Urgent action is needed to stop wounds getting worse.




A pressure wound that does not heal is a serious health risk. Early management is important to prevent pressure wounds from progressing.
Ask the person:
Do you have any pressure wounds?

If a person has a pressure wound advise them to avoid any pressure on the wound.
Refer to a health care professional for wound management.
Question
An older person is frail and unwell. They have been lying in bed, and find it hard to change position. They tell you they have a pressure wound on their hip.
What actions can you take?
All are correct
All four are steps that should be taken.
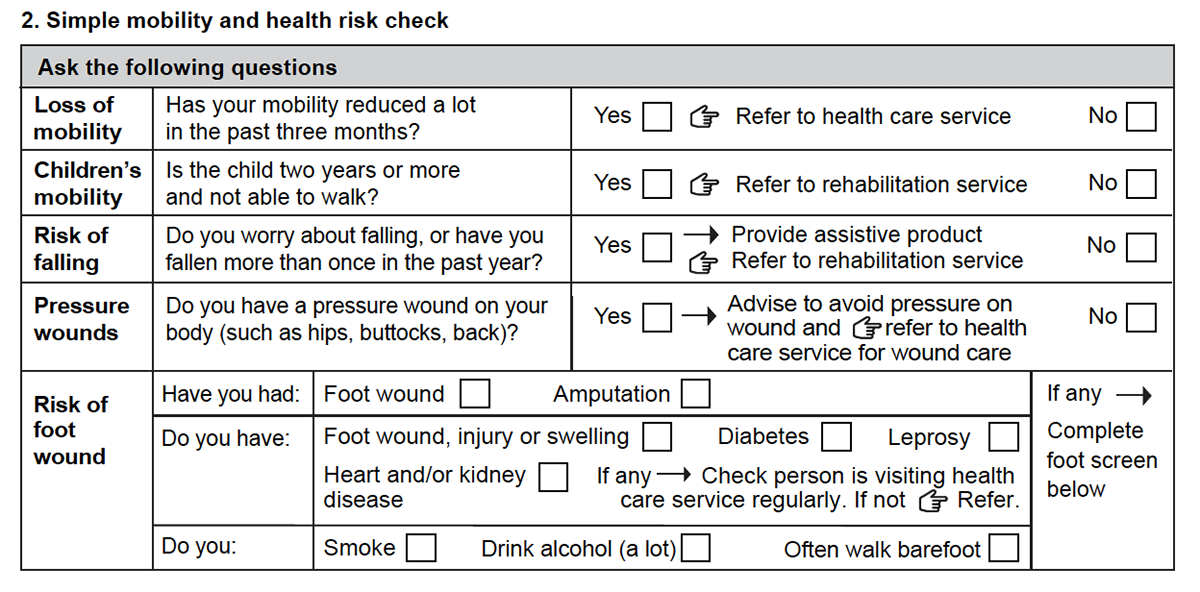
Risk of foot wounds
Use this part of the mobility screening form to decide if a foot screen is needed.
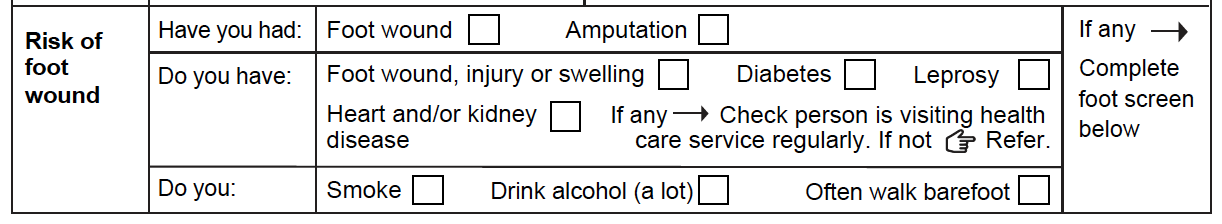
Ask the person:
Have you had a foot wound or amputation in the past?
Any person who has had a foot wound or amputation in the past, particularly if it took a long time to heal, is at risk of developing another foot wound.
Always complete a foot screen for a person who has had a foot wound or amputation in the past.
Ask the person:
Do you have:
- Diabetes,
- Leprosy,
- Heart and/or kidney disease
- A wound, injury or swelling on your foot.
People with diabetes, leprosy, heart and/or kidney disease are at risk of a developing a foot wound.
Always complete a foot screen for any person with these conditions or who has a wound, injury or swelling on their feet.
Ask the person:
- Do you smoke?
- Do you drink alcohol?
- Do you often walk barefoot?
Smoking and drinking a large amount of alcohol can increase the risk of a person having a foot wound as well as the length of time it takes for a foot wound to heal.
Walking barefoot increases the risk of a foot wound as the foot is less protected.
Always complete a foot screen for a person who smokes, drinks and/or walks barefoot often.
Question
Jensen is 60 years old. He can stand and walk, but feels unsteady at times. He is worried about falling.
Jensen has diabetes. He tells you that a year ago he cut his foot on a rock and the wound took a long time to heal.
Should you carry out a foot screen with Jensen?
Yes, carry out a foot screen. Also check Jensen is visiting his health care service for diabetes regularly.
If not, refer.
In the next topic you will learn how to carry out a foot screen.